Our Courses
First aid courses are training in the urgent performance of therapeutic and prophylactic actions necessary in accidents, sudden illnesses and measures of urgent assistance to wounded or sick people.

First aid training for the public is very important around the world.
Over a century and a half of history, hundreds of millions of volunteers around the world have saved lives in natural disasters, armed conflicts, and other life-threatening situations.
Do you know how to save the life of a loved one?
No one ever knows when and where an emergency will happen. It doesn't matter if it's a heart attack or a deep cut on the hand. It does not matter who the victim is, it can be an elderly man with a stroke, or a driver involved in an accident on a slippery road. No one is safe from harm.
We will not teach you how to avoid an accident (although we will give you some valuable tips), we will teach you how to keep an injured person alive until the ambulance arrives.
We will show you simple and effective first aid techniques, we will make sure you know how to help yourself and those around you.
Our News
Instructor-teacher

Elizabeth Poole
Anesthesiologist

Paul Mann
Cardiac resuscitation paramedic of the ambulance team

Eduardo Painter
Therapist

Bill Gordon
Emergency physician
Every State does everything possible to ensure the safety of its citizens: emergency services, ambulance, fire department, law enforcement. But not always these services can miraculously turn up where they were not called beforehand. Life is full of surprises and unforeseen situations:
- a traffic accident;
- a fire;
- an act of terrorism;
- a fight;
- numerous water accidents.
Often, when we watch news reports like this, we wonder, "Why didn't the people standing around help out? Could these "gawkers" have done anything other than record on a mobile device and then post the scoop on the Internet? But could we have done something about it ourselves? The desire is there, the strength of spirit is present, but often people lack knowledge. A first aid course will give you the opportunity to save someone's life. We want to share this so that in the future you will be able to provide real help to the injured. You don't need to graduate from medical schools or universities, and we don't recommend medications, injections or pills. All you have to do is make sure that the victim is able to wait for help from qualified professionals. When the ambulance arrives, you will be able to familiarize the doctors with the situation, thus guiding them on what to do next.
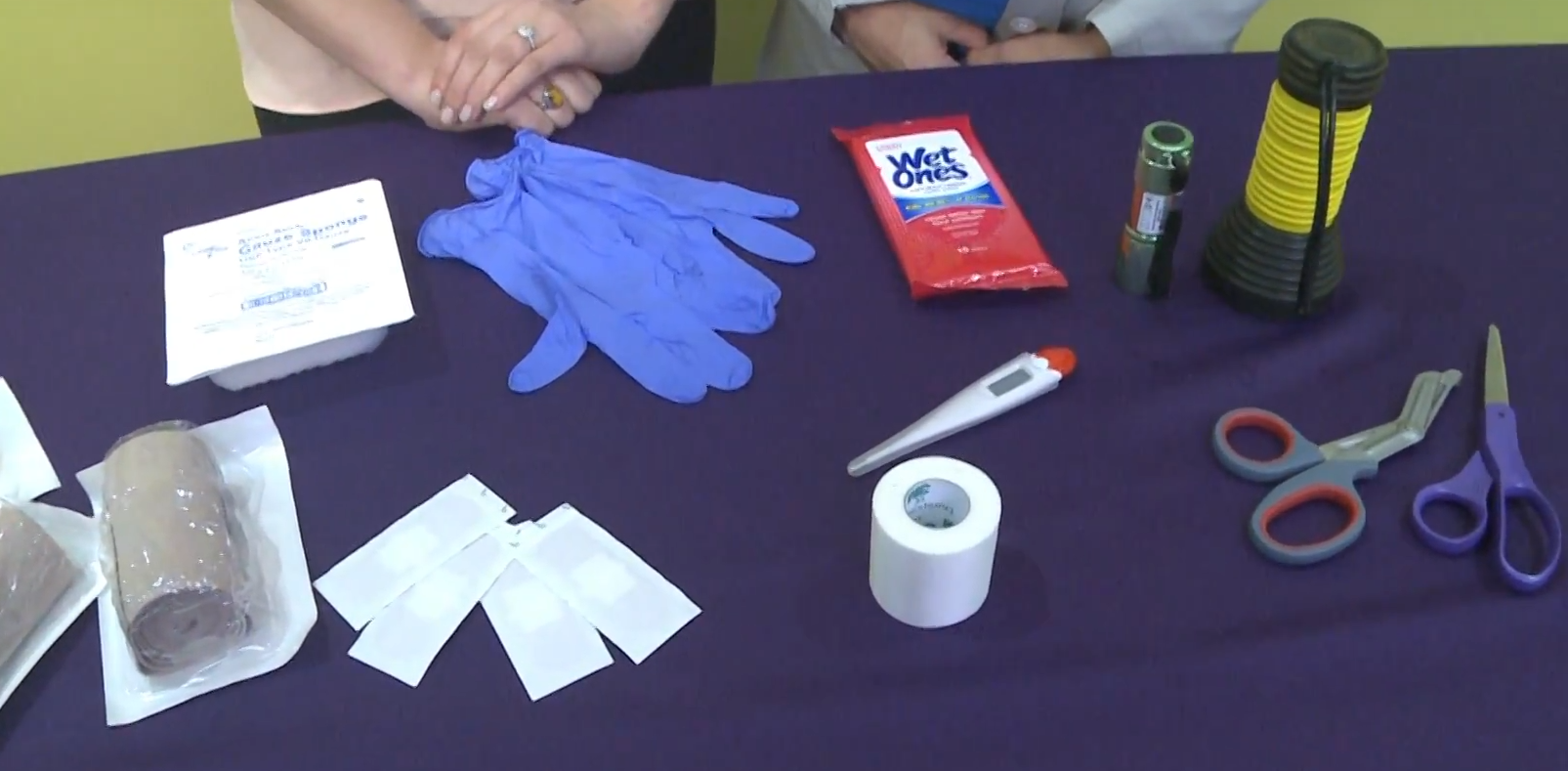
During our first aid courses we use various teaching aids:
-educational films;
-lectures that provide basic theory;
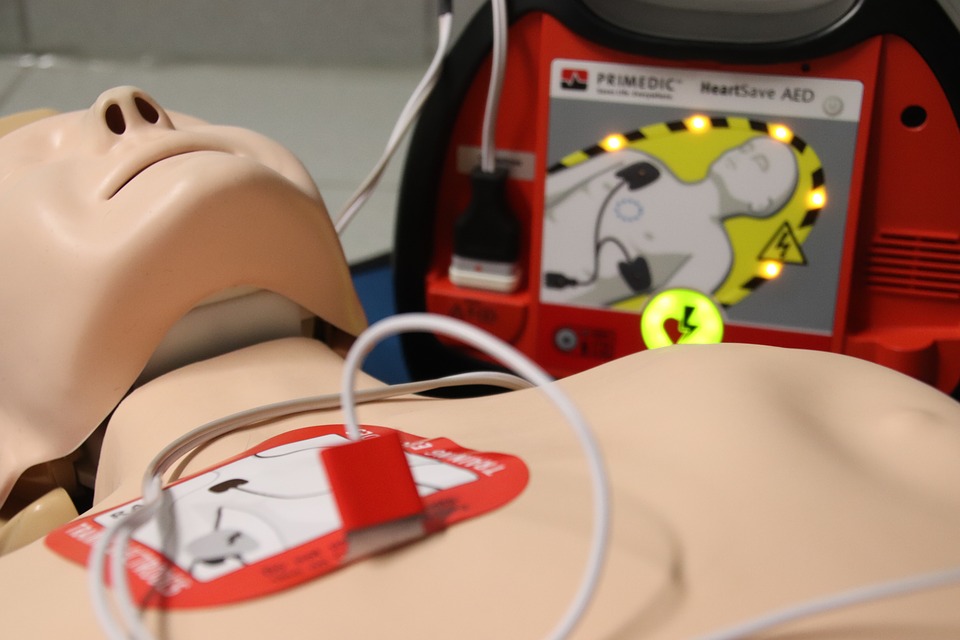
-Practical hours using dummies and other necessary equipment;
-You will be able to take a test at the end.
After our first aid courses you will be able to apply a splint correctly, stop bleeding with a tourniquet, perform CPR, and come to the aid of a fracture or dislocation. You will learn how to restore breathing and circulation before intensive care arrives.
This political situation requires skills today that can come in handy in a combat zone as well. We will look at various cases such as: a mine blast, shelling, and shrapnel wounds. We will tell you how and where to evacuate a wounded person, how to make an initial examination in such conditions and ensure that the wounded person has free air passage. In a terrorist attack, you will learn how to identify casualties who need immediate assistance and those who only need simple support.
Very important in a car accident is getting the victim out of the car. With a fractured cervical vertebrae or spine, improper evacuation can be fatal and instead of helping, you will only make things worse. In this course on fire safety behavior, we will tell you how to behave, what to watch out for, how to properly use fire extinguishers and what fire extinguishers are. What to do if your car catches fire. We will acquaint you with the main principles of evacuation from various buildings. If you would like to practice the skills you've been taught, we can offer you a Field Course in which real life situations will be enacted. In this scenario you will test your newly acquired knowledge and your psychological preparedness.
Emergency Situations at Home
The most painful times for people are when help is needed for loved ones. Children take care of their elderly parents and parents take care of their beloved children. We can help you figure out the first signs of a stroke, help with a heart attack, a heart attack. Very often this can help a person not to remain paralyzed for the rest of his life. In the very first minutes, while the body is still trying to fight and doctors are still on their way, you can save your loved one not only from death, but also from disability, which for some is worse than death.
First aid courses for children are needed not only for parents, but also for babysitters, teachers, educators, teachers and coaches. A child's body is different from an adult's. His bones are not as strong, his skin is much more delicate. A child recovers faster than an adult, but first aid plays a very important role in preventing disability, chronic pain or death. from First Aid Courses you will learn not only what to do when you have sprains, fractures, bleeding, bruises and burns, but also about first aid for animal bites (dog, spider, tick, wild animals), which can cause unforeseen consequences in the form of infection, rabies, poisoning.
In addition to these scary situations, you will also gain the necessary knowledge about everyday occurrences such as:
-high fever and fever;
-Vomiting and dehydration;
-cramping;
-stomach poisoning;
-respiratory distress due to a foreign body in the airways.
You will learn not only how to provide first aid, but also how to
clearly communicate the situation to ambulance personnel, which is
extremely important. At the end of these first aid courses, you will
receive a certificate. The duration of each course is 1 or 2 days
maximum. We will give you theoretical and practical knowledge. We will
help you acquire the determination that will not let you get confused in
an unforeseen situation. You will feel more confident about the future.
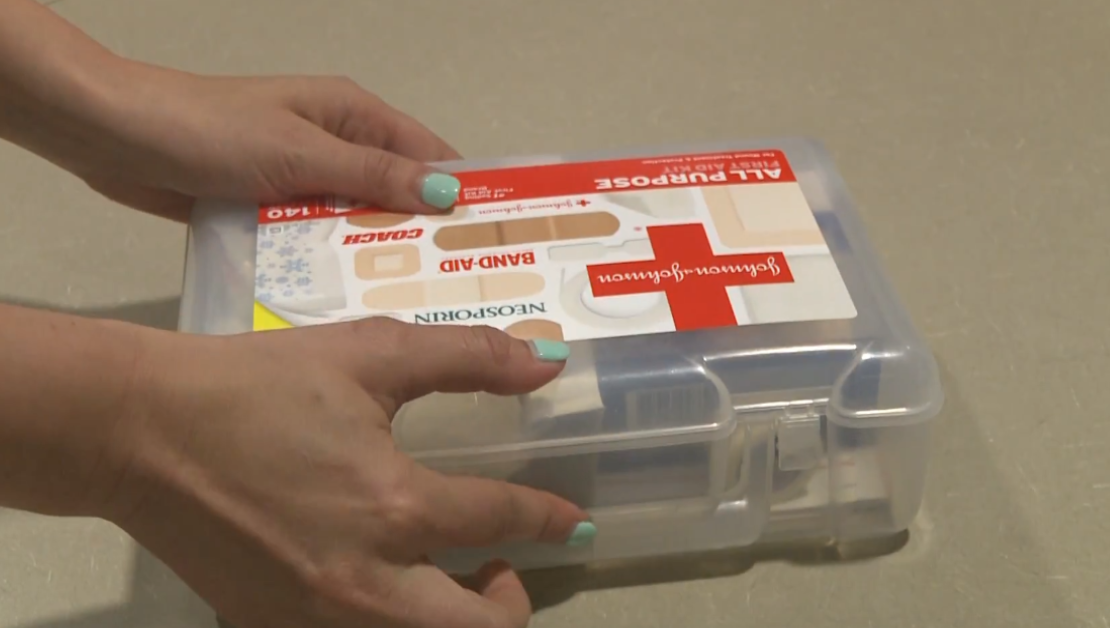
In addition to emergencies, you can even learn the rules of
completing a first aid kit for home, work, car, camping or just everyday
that you can carry in your bag. You will become a savior for yourself,
your loved ones and strangers who find themselves in trouble and will be
grateful to you for your skill, compassion and kind heart for the rest
of his life! First aid courses are designed for a small number of
people. This gives you the opportunity to work with everyone, to explain
things you don't understand, to work through them, and to improve them.
If you want to get such knowledge from professionals, contact us. We
are glad to everyone who decided to take such a step!